ONE HEALTH OKLAHOMA
One Health Initiative
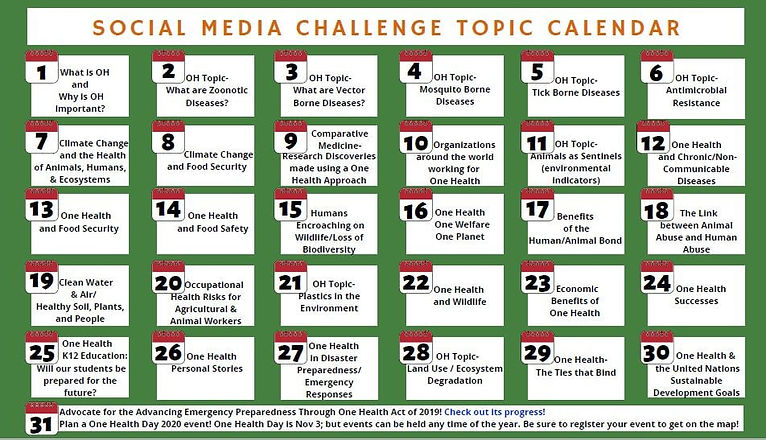
ONE HEALTH AWARENESS MONTH 2020
January 1, 2020
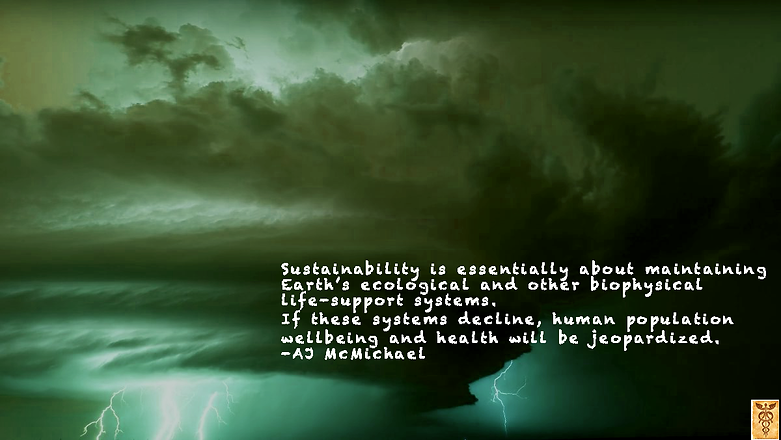
We still have only a very limited understanding of most aspects about our planet. Answering questions about this is essential for understanding the mechanistic role it plays on other scientific processes, and for developing tools to further explore this research avenue with more sensitive measurements and improved data collection.
THE TRIAD: HUMANS-ANIMALS-ENVIRONMENT
January 3, 2020
Day 3 of One Health Awareness Month. The triad of One Health, "Humans, Animals, and the Environment", is more important today than it was in 2009. We impact our environment daily, as it does us. Upward climate changes increase the frequency of emerging and reemerging infectious diseases. We know that up to 75% of infectious disease originated in animals, resulting in a "spillover event" to humans. It's our purpose and job to find out why, how, and where these may occur in the best interest of Public Health. From there we might find effective new treatments but finding "the cause" proactively rather than reactive is ultimately the better course of action.

MOSQUITO-BORNE DISEASES
January 4, 2020
Here in the US, most of us have local concerns of West Nile Virus and Zika virus, but little attention is given to Chikungunya virus (115 travel related cases in in US), Dengue virus (1,102 travel related; 14 autochthonous in US), Eastern Equine Encephalitis, (<10 in 2019), Malaria (1500 travel related cases in 2015), and Powassan virus (12 cases in 2019). There are many others of course. With increasing temperatures globally, we expect a northern expansion of the Aedes and Asian Tiger mosquito populations and with them come mosquito-borne diseases. #onehealth

ONE HEALTH MONTH DAY 6: ANTIMICROBIAL RESISTANCE.
January 6, 2020
Antibiotics have been overused in the human, animal, and environmental sectors for decades.The inability to treat bacterial diseases due to resistance to antibiotics from its indiscriminate use is a major public safety issue.
In 2015, the WHO initialized the Global Antimicrobial Resistance Surveillance System to:
-improve awareness and understanding of antimicrobial resistance;
-strengthen knowledge through surveillance and research;
-reduce the incidence of infection;
-to optimize the use of antimicrobial agents; and
-develop the economic case for sustainable investment that takes account of the needs of all countries, and increase investment in new medicines, diagnostic tools, vaccines and other interventions.
The WHO organization's recently issued a policy statement, recommending that farmers and the food industry stop using antimicrobials routinely to promote growth and prevent disease in healthy animals.
https://www.ncbi.nlm.nih.gov/pubmed/30700019
#onehealth #antimicrobialresistance
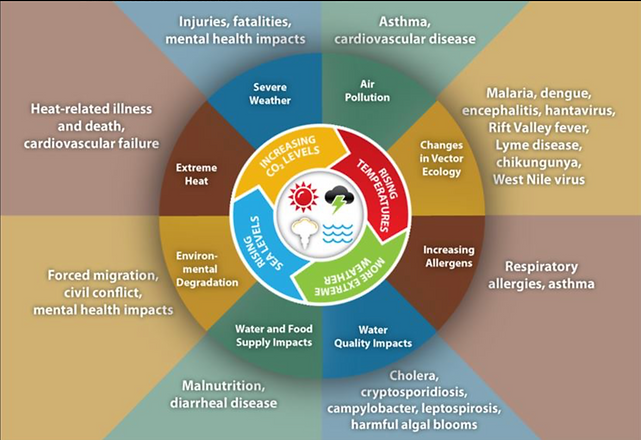
ONE HEALTH AWARENESS DAY 7: HEALTH AND CLIMATE CHANGE
January 7, 2020
I
Since 1988, the IPCC (Intergovernmental Panel on Climate Change) has looked at the human health risks associated with overall climate changes from weather extremes. Those weather extremes affect humans and animals directly due to thermal stress (temperature extremes) and flooding (rainfall extremes), and indirectly through changes in the ranges of disease vectors (mosquitoes, rodents, bats, etc), water-borne pathogens (contamination), water quality (sanitation and hygiene), air quality, and food availability and quality. These traumatic, infectious disease, nutritional, and psychological consequences
That vulnerability to infectious disease (especially vector-borne) is currently observed with the increased frequency of outbreaks also associated with rising temperature and rainfall patterns. When coupled with human population density and movement, migration patterns of animals outside their usual habitat (increased potential for zoonotic “spillover” events), forest clearance and land-use patterns (Amazonia; general urbanization), and biodiversity losses (animal population variability) we become more susceptible to disease.
What policy decisions and adaptation strategies need to be made?
#onehealth

ONE HEALTH AWARENESS DAY 8: ONE HEALTH AND FOOD SECURITY
January 8, 2020
As water supplies are reduced due to rising temperature and water quality is affected in extreme weather conditions, the food and agriculture industry is affected-we and animals are obviously linked. The food industry uses more than 70% of the world’s fresh water to grow the food we eat, feed livestock, and process that food. As our population increases, that global demand is expected to increase another 30% over the next 30 years.
Critical issues to address:
1. Only ~50% of these companies are actively forming a strategy. Not enough.
2. Continue with water risk assessments (water scarcity, water pollution (reduce microbial contamination; residual pesticides in water supply), reducing agricultural water run-off, impaired ecosystems, and improve water quality (especially after significant flooding) while addressing regulatory risks and concerns of shareholders
3. Support sustainable farming practices
4. Incentivize sustainable agriculture. Maintain soil health for agricultural resilience to weather extremes (drought, flooding, etc)
Forever #onehealth
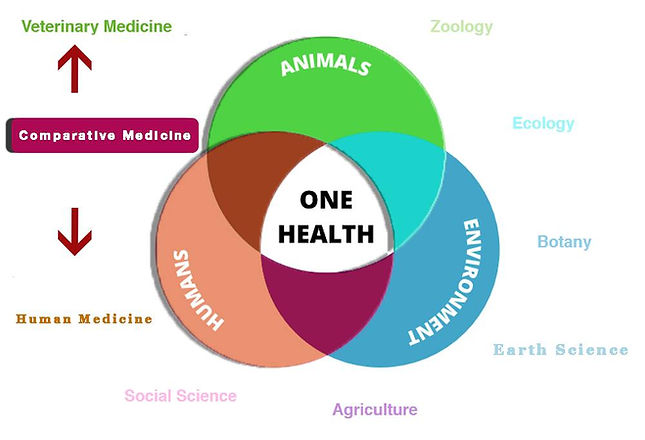
ONE HEALTH AWARENESS DAY 9: COMPARATIVE MEDICINE: RESEARCH DISCOVERIES USING A ONE HEALTH APPROACH
January 9, 2020
As a background, Comparative Medicine is a discipline composed of basic science researchers and veterinary clinician scientists that experimentally compare the similarities and differences between human and animal diseases. How does one disease “spillover” to humans? What is the difference between animal and human physiologic response to a pathogen? From that basic science bench, the results are then studied to see if they translate to improving health outcomes (Translational Medicine).
Some examples include:
1. Genetic variation in glioblastoma, breast, and prostate cancers
2. Reduction of Bovine tuberculosis and brucellosis transmission to humans
3. Type 2 diabetes in cats and humans
4. Obesity related complications in animals and humans
5. Improvement of adenoviral vectors for canine melanoma
6. Viroimmunotherapy for malignant melanoma
7. Immunotherapy with HER2-expressing L. monocytogenes for pediatric osteosarcoma
8. Regulatory requirements regarding clinical use of human cells, tissues, and tissue-based products
9. One medicine: a development model for cellular therapy of diabetes
10. Novel filovirus risk in New World bats
Reference:
Stroud C, Dmitriev I, Kashentseva E, Bryan JN, Curiel DT, Rindt H, Reinero C, Henry CJ, Bergman PJ, Mason NJ, Gnanandarajah JS, Engiles JB, Gray F, Laughlin D,
Gaurnier-Hausser A, Wallecha A, Huebner M, Paterson Y, O'Connor D, Treml LS,Stannard JP, Cook JL, Jacobs M, Wyckoff GJ, Likins L, Sabbagh U, Skaff A, GulAS, Hays HD, LeBlanc AK, Coates JR, Katz ML, Lyons LA, Johnson GC, Johnson GS,O'Brien DP, Duan D, Calvet JP, Gandolfi B, Baron DA, Weiss ML, Webster DA, Karanu FN, Robb EJ, Harman RJ. A One Health overview, facilitating advances in
comparative medicine and translational research. Clin Transl Med. 2016 Aug;5(Suppl 1):26. doi: 10.1186/s40169-016-0107-4. PubMed PMID: 27558513; PubMed Central PMCID: PMC4996801.
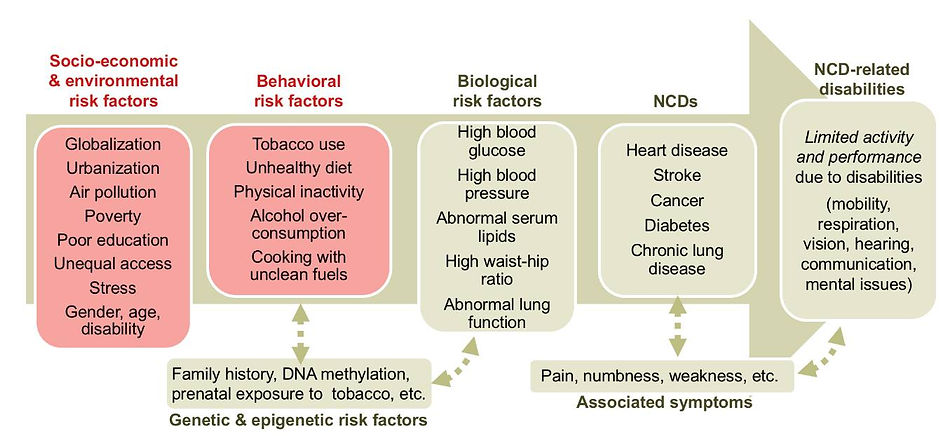
ONE HEALTH AWARENESS DAY 13: ONE HEALTH NON-COMMUNICABLE DISEASE
January 13, 2020
One Health Awareness Day 13: One Health Non-communicable Disease
Where does the One Health Environment-Animals-Humans triad concept begin with the discussion of non-communicable/chronic disease fit? We have discussed infectious disease and transmission in the One Health approach. Chronic diseases such as respiratory, cardiovascular, neurological, and metabolic diseases, obesity, diabetes, and cancer are linked to toxins i our environment. Multifactorial diseases often emerge in organisms whose defense capacities have been reduced by changes in nutrition, temperature, salinity, pH, exposure to pollutants, toxins, sanitation, and radiation have cumulative long-term effects (Destoumieux-Garzon, et al 2018). Environmental stress/pollution is a global concern.
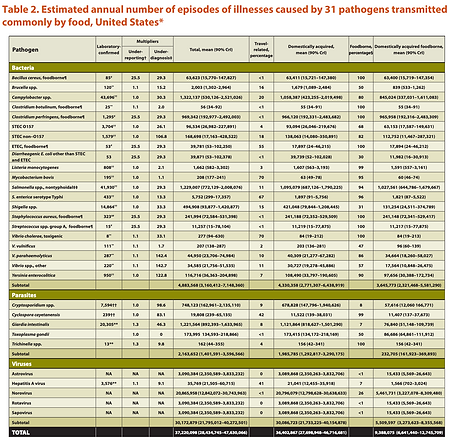
ONE HEALTH AWARENESS DAY 14: FOOD SAFETY
January 14, 2020
“In the modern world, bacteria and viruses travel almost as fast as money. With globalization, a single microbial sea washes all of humankind. There are no health sanctuaries.”-WHO
Food-borne illnesses are significant, costly, and a global problem. The global human population in 2019 exceeds 7.7 billion and by 2050, the world population is estimated to be over 9.7 billion. An estimated 30 billion food animals were produced to help feed this population and meet its growing demand for protein from animal sources King et al 2008). “Ensuring safe, accessible, affordable, and nutritious food is increasingly difficult, especially in a global context. Central to this challenge is the development of a One Health strategy and a new level of thinking and acting”.
It is estimated 48 million people suffer from food-borne illness, 128,000 are hospitalized, and 3,000 die each year (CDC). Of than more than 250 pathogens, 58% are caused by norovirus, Salmonella (11%( Clostridia perfringens (10%), Campylobacter jejuni (15% hospitalizations), Toxoplasma gondii (24% hospitalizations), and others. Potential pathogens include adenoviruses, sapoviruses, saffoldviruses, and picobirnaviruses (REF: FoodNet). Antimicrobial resistance adds to this problem.
New challenges to food safety will continue to emerge, largely because of:
* Changes in our food production and supply, including more imported foods.
* Changes in the environment leading to food contamination.
* Better detection of multistate outbreaks.
* New and emerging bacteria, toxins, and antibiotic resistance.
* Changes in consumer preferences and habits.
* Changes in the tests that diagnose food-borne illness.
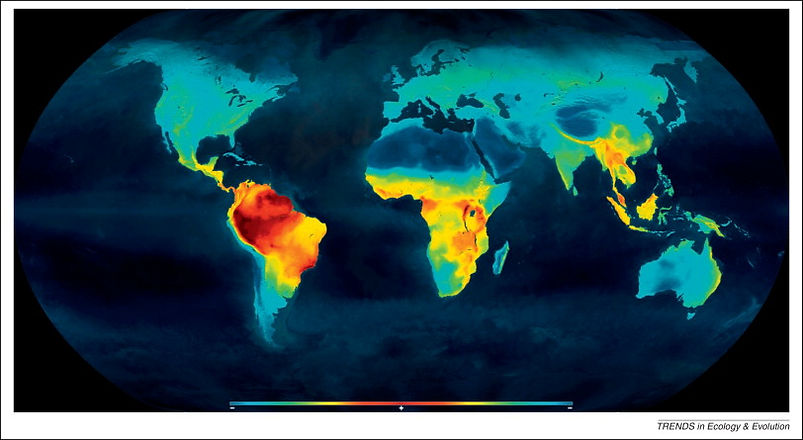
ONE HEALTH AWARENESS DAY 15: HUMAN ENCROACHMENT ON WILDLIFE: LOSS OF BIODIVERSITY
January 15, 2020
Biodiversity has had several definitions since 1916, but in general, that term reflects the variability of life and the density of it. 90% of the worlds species are located in the tropics. From the equator to the poles exist a latitudinal gradient of biodiversity. In the history of the world there have been 5 mass extinctions, the last one 65 mya. Following each mass extinction, there has been an increase in biodiversity (loss of natural selection) and many feel we are on the fringe of the sixth mass extinction: The Holocene Extinction.
Over the last 200-300,000 years humans as we know them have been in existence, our population has grown. Humans have only one natural predator: Humans. As such our population growth has created multiple biodiversity hotspots where an endemic species has experienced habitat loss. The majority of these biodiversity hotspots are in the forested regions in the tropics (e.g. Amazonia).
What is the impact of biodiversity loss have on human health?
Climate change are associated with change in biodiversity (changes in populations and distribution of disease vectors, scarcity of fresh water, impacts on agricultural biodiversity and food resources etc.).
-Increased demand for, and lack of, drinkable water
-Food safety
-With infectious disease, the vectors that survive are the ones that transmit the disease. With endemic species loss, the spread of infectious disease is greater leading to further loss of biodiversity.
-80% of the world’s population depends upon medicine derived from nature. With the loss of biodiversity, options are limited (antibiotic resistance).
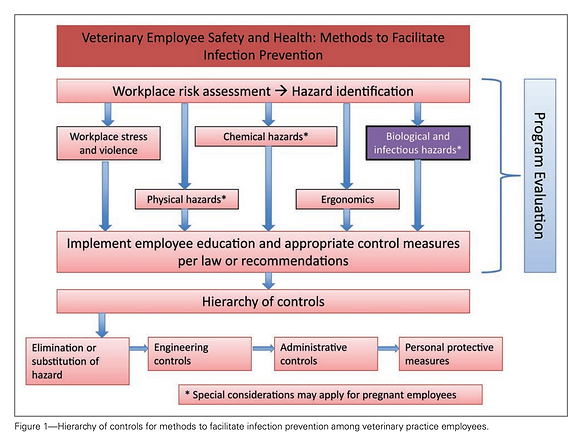
ONE HEALTH AWARENESS MONTH DAY 20: OCCUPATIONAL HEALTH RISKS FOR AGRICULTURAL AND ANIMAL WORKERS
January 20, 2020
The current standards here in the US to protect agricultural workers from injury and health risks are within General Industry (29 CFR 1910) and Agriculture (29 CFR 1928) in OSHA. Topics included are Grain Bins and Silos, Heat protection, protections from hazardous pesticides and the chemicals, respiratory diseases, unsanitary conditions, and general physical injury protection from falls, vehicle accidents, misuse/use of hazardous equipment and machinery.
As for Animal Workers, these General Industry Standards (29 CFR 1910) also apply, with special emphasis on protection from zoonotic diseases, safe handing standards, etc. The State regulation for importing animals is covered under 9 CFR 93, Chapter 1, Subchapter D and specifically in the Compendium of Veterinary Standard Precautions for Zoonotic Disease Prevention in Veterinary Personnel (Veterinary Infection Control Committee 2015). Since emerging viruses and spillover events are zoonotic in origin, strict adherence to these regulations and safety guidelines not only protects the health care worker but also protect the general public should an animal worker become infected and capable of transmitting disease to the general public. Examples include Material Safety Data Sheets (MSDS) are readily accessible to all workers, safe cleaning with potentially toxic chemicals, noise reduction, proper handling and disposal of objects that come in contact with an animal’s bodily fluid, bit protection, and wash station.
Understanding animal behavior is a major aspect to the prevention of transmission of disease. We don’t act as we usually do, and animals don’t either.

ONE HEALTH AWARENESS DAY 21: PLASTICS IN THE ENVIRONMENT
January 21, 2020
We seem to embrace plastic versions of Mount Trashmore globally-even as high up as Mount Everest-since 1907. During World War II plastic production increased by 300% since natural resources were diminished, leading to a greater demand for synthetics. As time passed plastic (cheaper) versions of paper, glass, packaging, and even wood in furniture appeared.
By the sixties, the enthusiasm was was in this quote, “Ben…one word…Plastics” (The Graduate; 1968).
The problem is getting rid of the trash. It might take at least 1,000 years to decompose in landfills (we won’t know for another 900 years, of course), those rapidly accumulating plastic bags in stores take at least 10-20 years to decompose, and 450 years for those water bottles we regularly use. Factors affecting degradation include chemical structure of the polymer, molecular weight, surface area, hydrophilicity/phobicity, and crystallinity [Ref: S Kubowicz , A Booth. Biodegradability of Plastics: Challenges and Misconceptions. Environmental Science & Technology 2017 51 (21), 12058-12060 DOI: 10.1021/acs.est.7b04051].
There are an estimated 79 million families in the US that probably can fill one of those 50 gallon recycle trashcans/month with plastic materials. So our annual volume of plastic recycle just might be as high as 5 x 10^10 gallons/year (50 gallons X 12 months X 79,000,000,000 families in the US). Then there is the accumulating mass of unconscious throw aways that end up as runoff in the ocean.
The scope of the problem includes:
-90% of seabirds and 50% of sea turtles have been found to have non digestible plastic in their gut. These nondigestible plastic chunks cause intestinal obstruction and perforations leading to death
-Wildlife become entangled in plastic debris
- Microplastics are associated with reproductive organ, liver damage, and thyroid dysfunction. For example, Bisphenol A, a compound used in plastics production, has been detected in 95% of adult human urine (National Report on Human Exposure to Environmental Chemicals). Detectable amount do not imply an adverse effect. It just means 95% of us have been exposed.
What is being done now?
We need to better understand the interaction of biotic and abiotic degradation
1. Develop technology towards microbial degradation of polymeric materials
2. Use biodegradable additives to allow increased microbial degradation

ONE HEALTH AWARENESS MONTH DAY 22: THE ZOONOTIC SPILLOVER EFFECT. ONE HEALTH AND WILDLIFE . A COMPARATIVE MEDICINE RESEARCH APPROACH
January 22, 2020
In the wake of the discovery of the Wuhan coronavirus in the news lately, this appears to be another spillover vent. Looking back into its relative, SARS, bats (mainly Rhinolophus; also Pipistrellus) seem to be the primary reservoir; palm civets and raccoon dogs are also known to harbor SARS.
So now we have yet another spillover event that has ties to a seafood wetmarket in Wuhan, China. Is there a connection with bats? Possibly, just like in Africa, bat bushmeat is not uncommon in Southern China, almost 43 species are hunted (Bats as bushmeat: a global review, Mickleburgh 2009; Exploitation of Bats for Bushmeat and Medicine, Mildenstein 2016).
Transmission does appear to be human-to human. Angiotensin Converting Enzyme 2 (ACE2) is the conserved human receptor for SARS-CoV S glycoprotein [Ren 2008]necessary to infect a human cell. So if we do what we usually do and compare the SARS S protein to the Wuhan coronavirus S protein, they are about 75% similar (using PDB structure sequences).
Inquiry Cover E-value %ID
6ACC_A 95% 0.0 75.12% (used in model)
5WRG_A 95% 0.0 74.04%
5X58_A 93% 0.0 76.01%
6NB6_A 93% 0.0 76.01%
6CRV_A 92% 0.0 75.78%
6CRW_A 92% 0.0 75.78%
In the S protein BD pocket (image shown), mutation at Asn-479 and Thr-487 in palm civet coronavirus seems necessary and sufficient for the virus to acquire the ability to efficiently infect humans.
In Wuhan coronavirus however, Asn-479 is replaced by Gln-493 (nonsynonymous) and Thr-487 is replaced by Thr-500 (synonymous). We don't know if that SARS Asn-479 to Wuhan Gln-493 affects infectivity but it might prove someday to be a monoclonal antibody target.
Then there might be the issue with protein disorder...time will tell.
ONE HEALTH AWARENESS MONTH DAY 23: ECONOMIC BENEFITS OF ONE HEALTH: A CHRONOLOGY OF THOUGHT FROM 2011-2019
January 23, 2020
Ruston et al 2011 [Economic benefits or drivers of a ‘One Health’ approach: Why should anyone invest?”]
-Why is One Health not main stream? Where are extra resource needed and who has control of the resources?
-If One Health is important, how can the case for a major paradigm shift be more persuasively
presented? Realize the dynamics of human population growth include expansion of livestock product and resurgence of transboundary zoonotic disease such that we recognize costs of disease in terms of losses in production of livestock, , the costs of controlling the disease , the human health impact costs. We need to look at avoidable costs by establishing efficient disease programs.
“In common with all the disease groups there is the need for an understanding of the role of human behavior in terms bringing host and pathogen together“.
2012
Between animal and human medicine there are no dividing lines—nor should there be.
-Rudolf Virchow, 1856
Häsler et al 2012 [The Economic Value of One Health in Relation to the Mitigation of Zoonotic Disease Risks]
The limitations of an economic approach are due to the necessary resources are not instantly available. The time investments and costs for training and to develop human, institutional, and infrastructure capabilities exceed initial fixed capital investment. There increasing demands on disease surveillance with new emerging and reemerging pathogens particularly with the aforementioned increased demand for livestock-derived food products, production intensity, and changes in geographic range of trade volumes. All these increase the risk of disease transmission. To emphasize that, look at the new coronavirus that arose from an unknown food source in a wetmarket in Wuhan, China as well as the use of bushmeat globally.
Economic assessments in three stages: 1) Strategic planning and outcome prediction; 2)Provide an interim assessment of the probability of a successful outcome and redirect funds towards that goal, and 3) Final analysis of the factors relevant to the success or failure and its economic value.
Narrod et al 2012. [A One Health Framework for Estimating the Economic Costs of Zoonotic Diseases on Society]
A stepwise approach is utilized:
1. Estimate the extent of the disease and potential spread; The impact and burden of disease (DALYs: years of life lost+years of life with a disability)
2. Estimate the cost of zoonotic disease on livelihoods outcomes (income, health, and trade), including environmental impacts; using cross-sectional data and compare cost of disease before and after interventions
3. Assess the cost-effectiveness of risk management strategies currently employed for reduction of human and animal zoonotic disease exposure risk; Direct costs and cost-effectiveness analysis
4. Identify factors affecting adoption of zoonotic risk reduction strategies in poor households, the commercial sector and government bodies. The KAPs: Knowledge; Attitude, and Perception Analysis; Willingness to Pay Analysis
Making One Health Operational (World Bank):
“What am I responsible for? (Classical approach)” or should it be, “What needs to be done? (Integrated Approach)”
2014
Häsler et al 2014 [A review of the metrics for One Health benefits ]
Benefits include
– protection of the environment and healthier ecosystems – enhanced social and cultural values
– improvements in human and animal health and well- being, and animal welfare
– better/improved/more effective/more rapid disease control and/or biosecurity measures
– a higher quality or quantity of information and data; more knowledge and better skills.
2016
Baum et al 2016 [Evaluating one health: Are We demonstrating effectiveness?]
“The absence of a standardized framework to capture metrics across disciplines, even in a generic format, may hinder the more widespread adoption of One Health among stakeholders.”
2017
Machalaba et al 2017 [One Health Economics to confront disease threats]
Key recommendations include: 1. systems thinking to identify risks and mitigation options for decision-making under uncertainty (hazard-specific); 2. multisectoral economic impact assessment to identify wider relevance and possible resource-sharing (opportunity costs of resources, financial consequence of zoonotic disease, post-analysis of benefits of prevention) and 3. consistent integration of environmental considerations (valuing ecosystem regulation of disease risk, the impact of mitigation measures on ecosystem
services, and the role of pathogens in regulating other ecosystem processes and services)
2019
Smith et al 2019 [Infectious disease and economics: The case for considering multi-sectoral impacts]
These involve the Health sector (e.g, Zika epidemic estimate costs $7-18 billion dollars), agricultural sector (50% livestock losses are from zoonotic disease); tourism and travel (SARS lost 41% international travel; H1N1 epidemic cost Mexico $2.8 billion dollars in pro and travel), trade and retail (SARS global economic loss=$40 billion dollars; Nipah virus $582 million dollars)
This is why we need ONE HEALTH.
ONE HEALTH AWARENESS MONTH DAY 24-ONE HEALTH SUCCESSES. A STRANGE CASE OF HUMAN RABIES
January 24, 2020
In the early 1990’s, there were more than 100 cases of human rabies-virtually all were lethal. From 1960 to 2018, only a total of 125 human rabies cases were reported in the United States, with 25% resulting from dog bites during international travel. Of the infections acquired in the United States, 70% were attributed to bats. This decline is most likely due to widespread pet vaccinations, effective post-exposure treatment and the relative rarity of undetected bites by rabid animals.
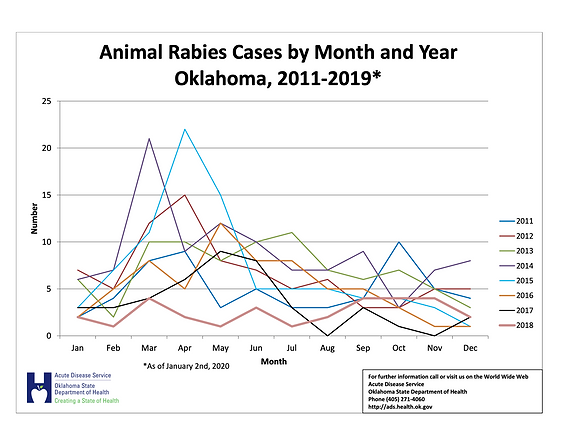
In Oklahoma in 2018, there were 30 reported cases of animal rabies. As of January 2020, there have been a reported 23 cases of animal rabies, with the majority found in skunks (see image). There seems to be a peak rise in the spring. Every spring skunks, raccoons, foxes, and bats become more active as they transition from winter to spring. This activity leads to interactions with cats, dogs, and humans and with it comes the risk of transmission.
As for a personal story, back in 1981, I was a full-time microbiology student at OU and worked full-time in the ER at South Community Hospital in Oklahoma City as an ER Tech along with Ben Potter (now DDS) , Marty Lopez (now MD), and Jay Cunningham (now DO). Pretty good company I’d say. Sandy Gilbreath was the nurse on duty. During that summer, I clearly remember this odd fellow that had the chief complaint of difficulty swallowing. No fever, but I do recall that he was a bit disheveled, anxious, and somewhat sweaty. He also asked for a cup of water but couldn’t swallow. A barium swallow was negative so it was felt to be just anxiety. He came in every day and progressively had difficulty breathing and was visibly agitated and a bit confused. Aspiration? Possibly. Anyway, he was always discharged from the ER, only to return the next day with worsening symptoms. On the following Saturday, he was brought in in full arrest and expired. The internist on duty, Dr. Fernando (?) reviewed his history and suggested a diagnosis of rabies.
He was right. A brain biopsy was positive for Negri bodies.
Needless to say, with all of us exposed to him over the course of 5 days, the CDC came in and there ere around 100 of us that had “significant” exposure to warrant post-exposure vaccination (HDCV). Luckily, none of us developed rabies.
Lesson learned, “There are more things in Heaven and Earth, Horatio, than are dreamt of in your philosophy.” That concept has always remained prominent in consideration of the differential diagnosis. When you hear hoofbeats, think of horses, not zebras. That said, unicorns don’t exist but zebras do.
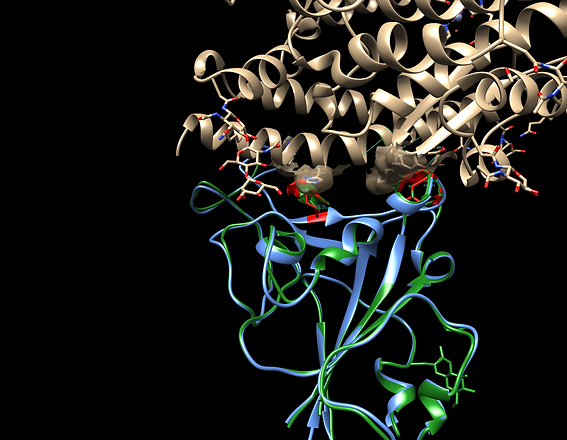
ONE HEALTH AWARENESS MONTH DAY 27: COMPARATIVE MEDICINE AND THE WUHAN COV SITUATION
January 27, 2020
What we may know from previous structural models is that mutation Asn-479 and Thr-487 in palm civet coronavirus seems necessary and sufficient for the virus to acquire the ability to efficiently infect humans. Does this apply to what we are leaning about how the Wuhan CoV can infect humans? In One Health, comparative medicine approaches are a necessary pre-evaluation tool. Granted, de novo, computer generated models can be inaccurate as they may not represent the true biochemical interaction. Still, it gives us a starting point. In the multiple sequence protein alignment, we do see less conservation in the C-terminus of the receptor binding domain that does contain the critical Asn-157 and Thr-165 residues that bind to human ACE2. From a surface comparison alone, the upstream Wuhan Gln-493 appears to have less surface contact with ACE2 His-34 than does SARS Asn-157 but does appear to have greater contact with Lys-31. Does it matter? Possibly. The SARS CoV asparagine (Asn) binding to histidine (His) is known to have a stronger biochemical interaction. We'll see.
ANIMAL RABIES IN THE SPRINGTIME.
February 10, 2020
Rabies is a serious threat to the health of humans and animals and is deadly when left untreated. As the temperature rises, the numbers of rabies cases increase as well. Bats do hibernate, so springtime is when wild baby animals are born and bats often return to the local area. The most common source of human rabies in the United States is from bats. For example, in the 19 naturally acquired cases of rabies in humans from 1997-2006, 17 were associated with bats. 14 had known encounters including six people with a history of handling a bat while removing it from their home. One person was bitten by a bat while releasing it outdoors after finding it on the floor inside a building. One person picked up and tried to care for a sick bat found on the ground outdoors. Three men ages 20, 29 and 64 had no reported encounters with bats but died of bat-associated rabies viruses (phylogenetic analysis).
Delays in diagnosis are common. The clinical features of rabies encephalopathy are highly nonspecific at the onset and clinicians from low endemic areas usually face difficulties in recognizing cases during the early stages (Chacko et al 2016). There may not be a history of an animal bite, especially from a bat. In 61% of human rabies cases due to bat rabies virus variants there is no history of a bat bite or scratch and in 34% of cases there is no known history of any “contact” with bats at all (DeSerres 2008). Bites can be so small they go undetected (as in this case)-See image below (defensive bite from a canine tooth of a silver-haired bat (Lasionycteris noctivagans). The differential diagnoses that were considered before a definitive diagnosis was made included panic disorder, tetanus, viral encephalitis, drug toxicities or withdrawal, CNS vasculitis, bronchitis with pleurisy, sepsis, viral encephalitis, cervical radiculopathy, muscle strain, lower back strain, esophageal spasms, dysphagia, anxiety, aseptic meningitis, Lyme meningoencephalitis with peripheral neuropathy, sinusitis, pneumonia, severe hyponatremia and atypical chest pain (Soun et al 2006).
What to do!
Bat-proof your home. Caulk openings larger than a 1/4-1/2 inch. Use window screens, chimney caps, and draft guards beneath doors to attics, fill electrical and plumbing holes with stainless steel wool or caulking, and ensure that all doors to the outside close tightly. Over all outside entry points [CDC Keeping bats out of your house].
Case History Example
Rabies Case Timeline (Utah 2018)
Probable exposure date 10/02/2020. Risk factors included recent grouse hunting trip, ownership of 2 dogs, and a horse; bat infestation (attic/living area) since August 2018; some removed from home with bare hands The Mexican free-tailed bat (Tadarida brasiliensis) is the most common host species detected in Utah (42%) followed by the Big Brown bat (Eptesicus fuscus; 21%) and the Silver Haired bat (Lasionycteris noctivagans; 15%). In Oklahoma, the Free-Tailed Bat (Tadarida brasiliensis( and the Big brown Bat (Eptesicus fuscus) are commonly found.
10/17/2018 55 y/o white male presented with chief complaint of neck and arm pain, presumably work related.
10/19/2018 ER with chief c/o neck pain with spasms, right arm paresthesias. Vital signs normal. Also c/o dysphagia. Discharged home on steroids
10/20/2018 ER again with c/o breath, tachypnea, lightheadedness , arm pain, and severe esophageal spasms. He became delirious and was admitted to the hospital
10/21/2018 Fever (104.7), respiratory failure requiring intubation, comatose. Presumed to be autoimmune encephalitis.
10/26/2018 Refractory seizures.
11/04/2018 Death
11/07/2017 CSF, serum, skin biopsy and saliva sent to CDC along with brain stem and cerebellar biopsy specimens.
Results: Rabies IgM +; Rabies IgG +; Rabies neutralizing antibodies found in serum (1:5,400; 43.2 IU/ml) and CSF (1:250; 2.0 IU/ml). Skin biopsies - for viral antigen.
Rabies virus antigen (nucleoprotein) and RNA was detected in postmortem brain stem tissue and cerebellum specimens by DFA and real-time RT-PCR.
Phylogenetic nucleoprotein sequence analysis was consistent with Tadarida brasiliensis rabies virus variant [accession numbers JN594500-JN594503; DQ445318-DQ445330; DQ445532 from Streicker et al 2012]
Symptoms of Rabies in Bats:
Weight loss, ataxia, and paresis
Particular bat species are associated with specific RABV variants (Mondul et al 2003 (Tables 6.2 and 6.3 shown)
References
Soun VV, Eidson M, Wallace BJ, Drabkin PD, Jones G, Leach R, Cantiello K, Trimarchi CV, Qian J. Antemortem diagnosis of new york human rabies case and review of u.s. Cases. Int J Biomed Sci. 2006 Dec;2(4):434-45. PubMed PMID: 23675013; PubMed Central PMCID: PMC3614649
De Serres G, Dallaire F, Côte M, Skowronski DM. Bat rabies in the United States and Canada from 1950 through 2007: human cases with and without bat contact. Clin Infect Dis. 2008 May 1;46(9):1329-37. doi: 10.1086/586745. PubMed PMID: 18419432.
Mondul AM, Krebs JW, Childs JE. Trends in national surveillance for rabies among bats in the United States (1993-2000). J Am Vet Med Assoc. 2003 Mar 1;222(5):633-9. PubMed PMID: 12619845
Chacko K, Parakadavathu RT, Al-Maslamani M, Nair AP, Chekura AP, Madhavan I. Diagnostic difficulties in human rabies: A case report and review of the literature. Qatar Med J. 2017;2016(2):15. Published 2017 Apr 21. doi:10.5339/qmj.2016.15
Peterson D, Barbeau B, McCaffrey K, et al. Human Rabies — Utah, 2018. MMWR Morb Mortal Wkly Rep 2020;69:121–124.
Streicker DG, Turmelle AS, Vonhof MJ, Kuzmin IV, McCracken GF, Rupprecht CE. Host phylogeny constrains cross-species emergence and establishment of rabies virus in bats. Science. 2010 Aug 6;329(5992):676-9. doi: 10.1126/science.1188836. PubMed PMID: 20689015.
https://www.cdc.gov/rabies/bats/management/index.html
Streicker DG, Lemey P, Velasco-Villa A, Rupprecht CE. Rates of viral evolution are linked to host geography in bat rabies. PLoS Pathog. 2012;8(5):e1002720. doi: 10.1371/journal.ppat.1002720. Epub 2012 May 17. PubMed PMID: 22615575; PubMed Central PMCID: PMC3355098.

